Stem Cells Unlock Genetic Cures—but Ethical Dilemmas Linger
Stem cells hold the key to treating diseases at their genetic source. These unique cells can self-renew and transform into specialized tissues, offering hope for conditions like sickle-cell disease. Yet their potential is matched by ethical debates, high costs, and uneven global regulations.
Stem cells are defined by two key traits: the ability to divide repeatedly and the potential to become different cell types. Embryonic stem cells, which can form nearly any tissue, remain controversial due to ethical concerns. In contrast, induced pluripotent stem cells (iPSCs) avoid these issues by reprogramming a patient's own cells, enabling precise disease modeling and personalized treatments.
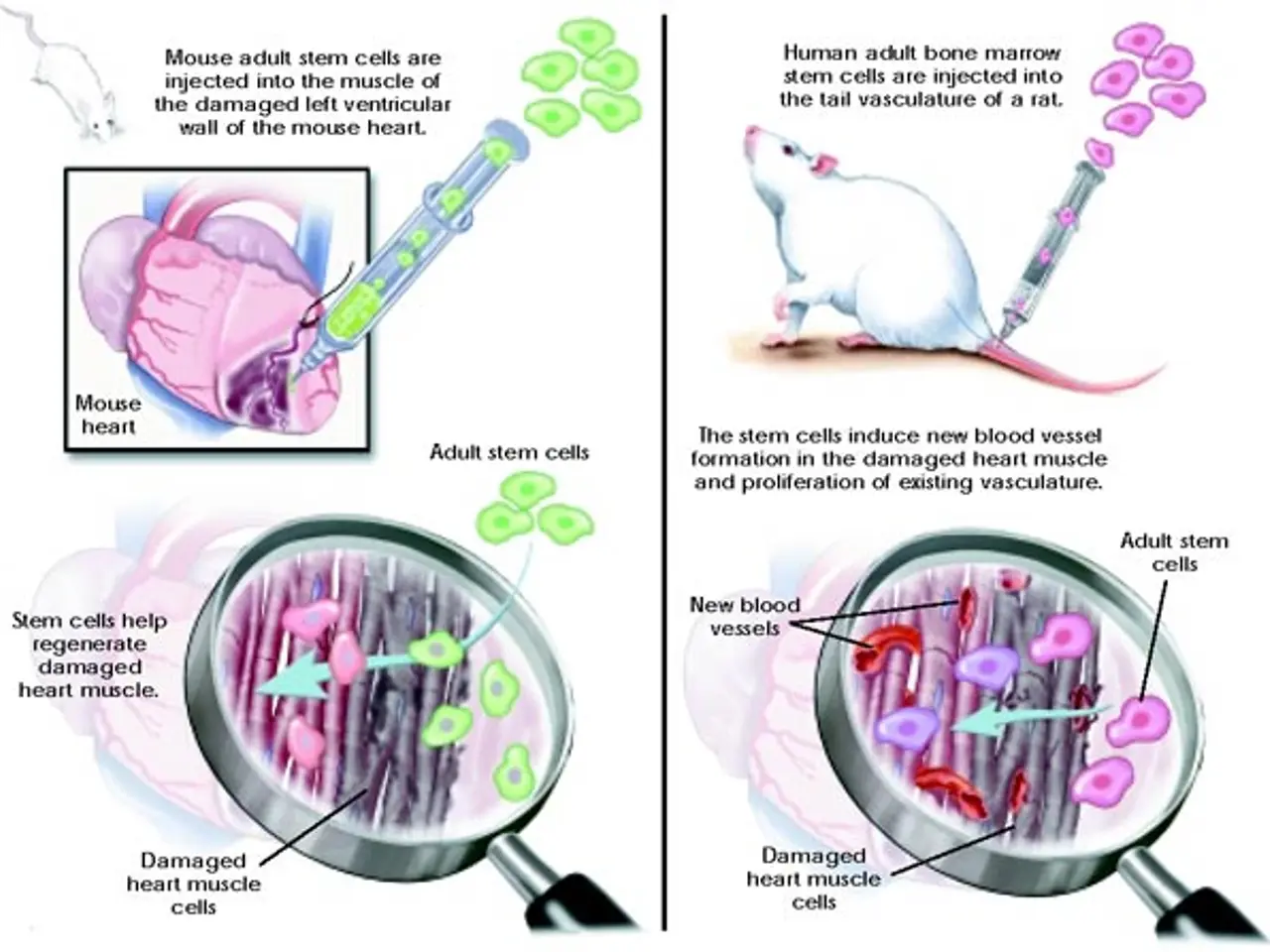
Adult, or somatic, stem cells have narrower potential but already support life-saving therapies. Bone-marrow transplants, for instance, rely on these cells to restore blood and immune function. Meanwhile, gene-editing tools paired with stem cells have successfully corrected genetic defects in sickle-cell patients, proving their power to tackle disease at its root. New technologies are expanding research possibilities. Organoids—miniature lab-grown organs—and organ-on-a-chip systems now offer alternatives to animal testing. These tools also help tailor treatments to individual patients. However, advances in creating embryo-like models for studying early development are raising fresh ethical questions about the definition of life and moral boundaries. Despite progress, major challenges remain. The high cost of stem-cell therapies risks deepening global health inequalities unless policies intervene. Unregulated markets, particularly in countries like Mexico and Saudi Arabia, leave patients vulnerable to exploitation by unauthorized clinics. Weak oversight in some African nations further limits access to advanced treatments like CAR-T cell therapy, while enabling unsafe practices.
The future of stem-cell science hinges on four critical improvements: stronger safety measures, lower costs, standardized production, and tighter regulations. Without these, the gap between cutting-edge treatments and those who need them will only widen. Addressing these issues is essential to ensure equitable access and prevent harm from unproven therapies.