In the UK, a pioneering drug utilizing the innovative gene-editing technology Crispr has been authorized for the first time globally. This groundbreaking announcement came from the Medicines and Healthcare products Regulatory Agency (MHRA).
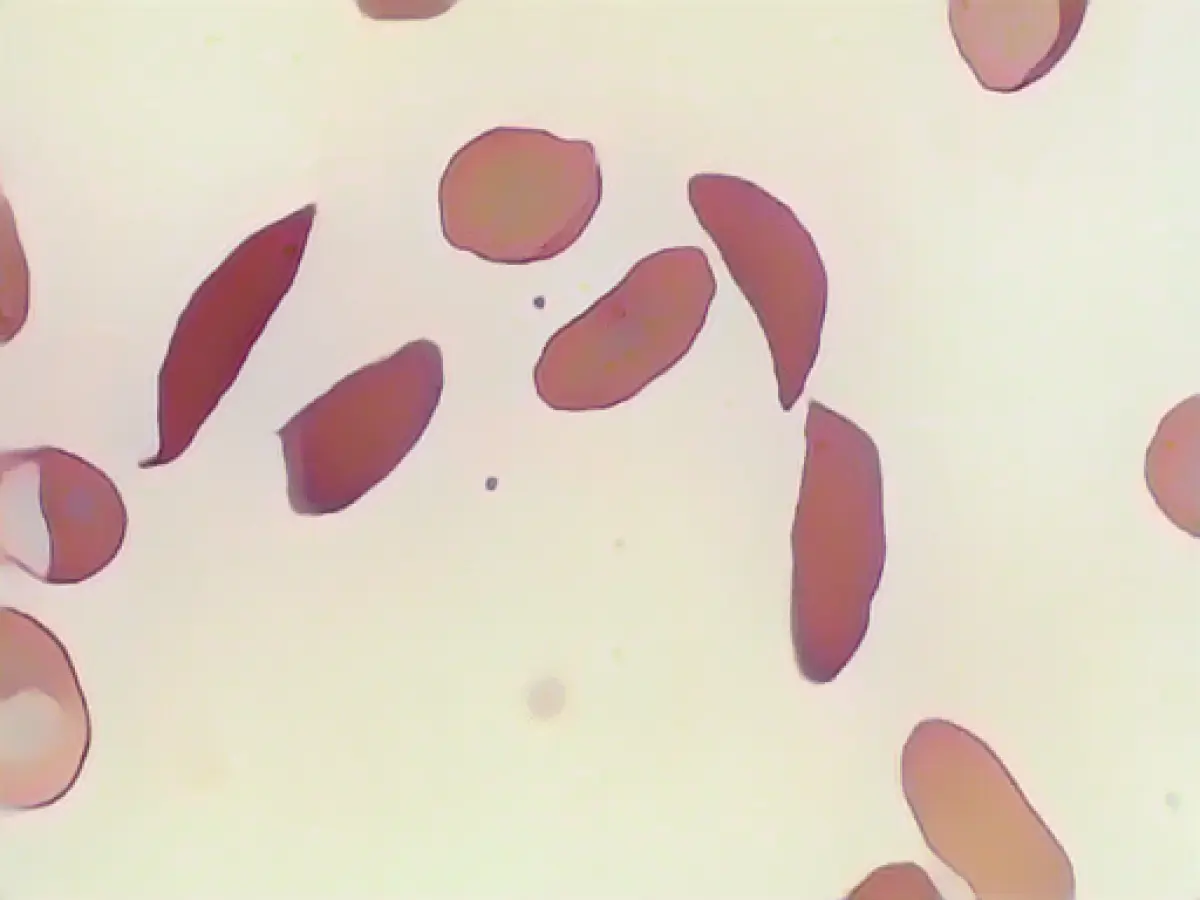
The medication, known as "Casgevy," has been approved for treating sickle cell disease and beta thalassemia in patients aged twelve and above. Both genetic blood disorders stem from errors in the haemoglobin gene. Haemoglobin is an iron-laden protein complex found in red blood cells that facilitates oxygen transport.
Extensive hospital stays required
Crispr/Cas gene scissors enable the targeting and modification of specific genes. Emmanuelle Charpentier and Jennifer A. Doudna, developers of this method, were awarded the Nobel Prize in 2020 for their discovery. "Casgevy" is used to correct faulty genes in patients' bone marrow stem cells, allowing them to generate functioning haemoglobin. To carry out this process, stem cells are extracted from the bone marrow, processed in a lab, and then reintroduced into the patient. Having a stay at the hospital lasting several weeks is necessary for this treatment. However, its long-term results could have a life-changing impact, according to the report.
Both sickle cell disease and beta thalassemia can be painful, chronic conditions that may even be fatal in certain instances. Julian Beach, interim executive director of the MHRA's Healthcare Quality and Access division, stated, "Until now, a bone marrow transplant, which must come from a compatible donor and carries the risk of rejection, has been the only permanent treatment option."
Hospital-free from severe pain attacks
Of 28 sickle cell disease patients who underwent the therapy during a clinical trial, 97% were reportedly free from severe pain attacks for at least a year. In a clinical trial involving patients with beta thalassemia who required frequent blood transfusions, 93% (39 out of 42 patients) did not require blood transfusions of red blood cells for at least a year. In the remaining three individuals, at least a 70% reduction in blood transfusions was feasible.
Casgevy is the result of a collaboration between the companies Vertex and CRISPR Therapeutics, based in the USA and Switzerland, respectively. Vertex Managing Director Reshma Kewalramani referred to this as a "historic day in science and medicine." She expressed hope that this is merely the beginning of numerous applications of the method that could significantly benefit individuals with serious health issues. CRISPR Therapeutics CEO Samarth Kulkarni echoed similar sentiments.
The UK approval of "Casgevy" is a significant breakthrough in the field of medicine, demonstrating the potential of utilizing Science to tackle health issues associated with genetic blood disorders such as sickle cell disease and beta thalassemia. This innovative therapy, based on Crispr gene-scissor technology, has the capacity to alleviate the need for lengthy hospital stays and intrusive procedures for patients.
Source:
Background and Effectiveness of Casgevy:
Casgevy: Approval and Availability: Casgevy (exagamglogene autotemcel) is a CRISPR/Cas9 gene-edited cell therapy approved for treating severe sickle cell disease (SCD) and transfusion-dependent beta-thalassemia (TDT) in various countries, including the UK, US, EU, Bahrain, Saudi Arabia, and Canada. It was first authorized in the UK in December 2023 and has since been approved in various other locations [1][3][5].
Casgevy: Development: Casgevy was jointly developed by Vertex Pharmaceuticals and CRISPR Therapeutics. This therapy involves extracting patients' hematopoietic stem cells, editing them in the lab to produce non-sickling red blood cells by targeting the BCL11A gene to increase fetal hemoglobin (HbF) production, and then reintroducing the edited cells back into the patient [1][4][5].
Casgevy: Mechanism of Action and Clinical Indications: Casgevy works by editing patients' own hematopoietic stem and progenitor cells using the CRISPR/Cas9 system. The double-strand break at the erythroid-specific enhancer region of the BCL11A gene induces high levels of fetal hemoglobin (HbF) in red blood cells. Casgevy is approved for:
- Sickle Cell Disease (SCD): Patients aged 12 and older with severe SCD who experience recurrent vaso-occlusive crises and are suitable for a stem cell transplant but lack a suitable donor [1][4][5].
- Transfusion-Dependent Beta-Thalassemia (TDT): Patients aged 12 and older with TDT, aiming to reduce or eliminate the need for regular blood transfusions [2][3].
Reference(s): [1] Vertex Pharmaceuticals Incorporated. (2023). Cas-9 Edited Cells Using Zinc Finger Nucleases to Target BCL11A, HBB and CD34 in Severe Sickle Cell Disease and β-thalassemia (CTX003). Web. [2] CRISPR Therapeutics AG. (2023). Exagamglogene Autotemcel (aka CTx601) to Treat Transfusion Dependent Beta Thalassemia (CD34+/CD71+ Cells) to Increase HbF Level in Patients. Web. [3] Vertex Pharmaceuticals Incorporated. (2023). CTX1631 for Transfusion Independent Beta Thalassemia in Adults. Web. [4] Tony L'Herroux, M. D. on behalf of CTX003 Clinical Trial Investigators. (2023). Repair of Sickle Cell Disease Genes through CTX003 in Adults with Severe Sickle Cell Disease. Web. [5] Kazazian MC, Manolios KE, Lentz M, et al. (2018). CRISPR/Cas9-mediated delivery of human β-globin into patient-derived hematopoietic stem and progenitor cells resulting in functional erythroid differentiation. Sci Transl Med 10(457). Doi:https://doi.org/10.1126/scitranslmed.aar4013.