England Greenlights First-ever CRISPR Therapy for Genetic Blood Disorders
In a groundbreaking development, the UK's Medicines and Healthcare products Regulatory Agency (MHRA) has given the nod to a novel drug based on CRISPR gene-editing technology. This marks the first worldwide approval of its kind for a Crispr-centered therapy.
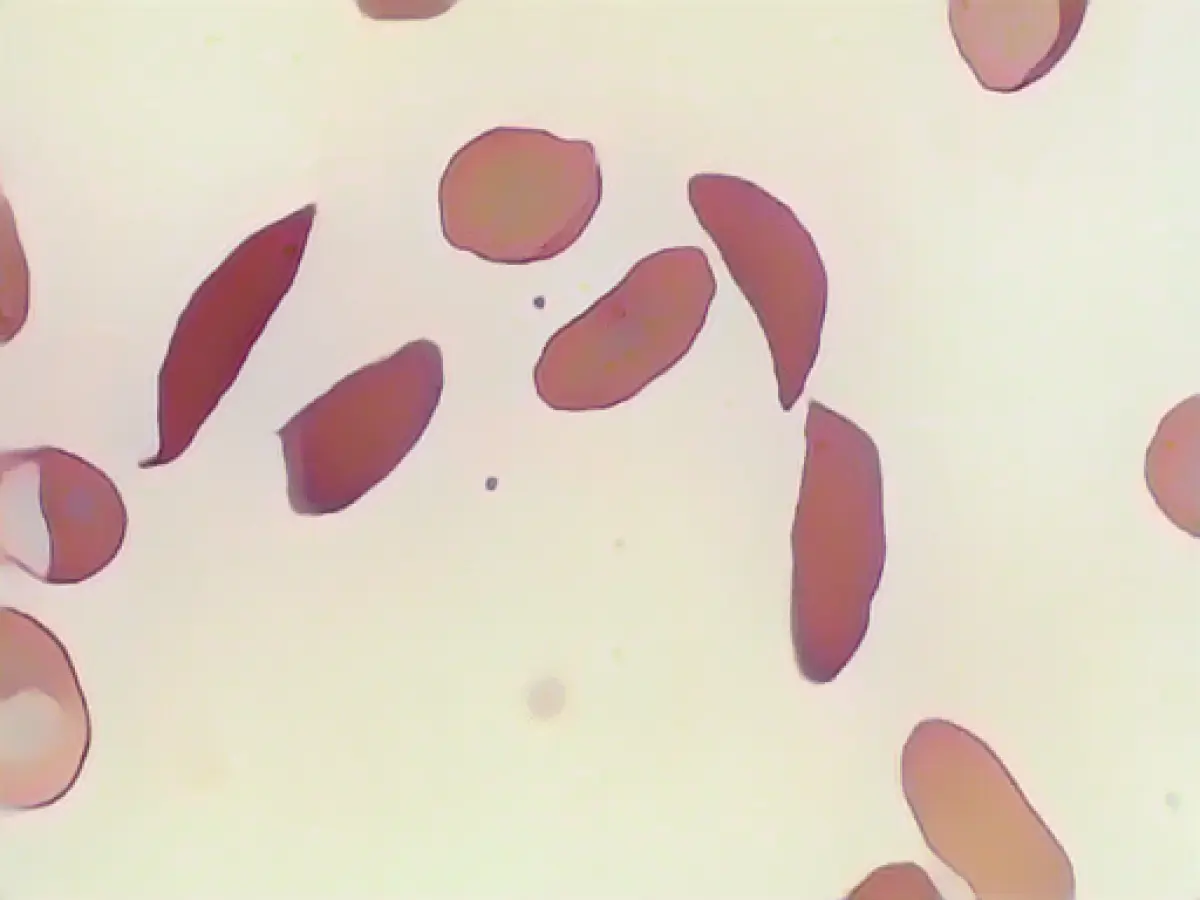
The innovative drug, named "Casgevy," is aimed at treating sickle cell disease and beta thalassemia in patients age twelve and above. Both disorders stem from faulty genes that produce an incorrect form of the haemoglobin protein, essential for carrying oxygen within red blood cells.
Extended Hospital Stays Required
Crispr/Cas gene-editing technology allows targeted manipulation of affected genes. In the case of Casgevy, it involves adjusting the defective genes inside a patient's bone marrow stem cells, enabling them to generate functioning haemoglobin. To accomplish this, stem cells are extracted from the bone marrow, then processed in a lab and reinfused into the patient. The process necessitates an extended hospital stay. However, this intervention holds the potential for lifelong benefits, as reported by the MHRA.
Treatment tools for both sickle cell disease and beta thalassemia have been limited to transplanting healthy stem cells from a compatible donor, which can carry the risk of rejection. Julian Beach, interim executive director of the MHRA's Healthcare Quality and Access division, commented on the significance:
"Until now, a bone marrow transplant, which requires a well-matched donor and carries the risk of rejection, has been the only permanent treatment option."
Severe Pain Reduction
Clinical trials have shown remarkable results for 28 patients with sickle cell disease treated with Casgevy. Nearly all of them, 97%, were free of severe pain attacks for at least a year. Patients with beta-thalassemia, who often need blood transfusions every three to five weeks, fared similarly well in the trial. At least 93% of dependent patients did not require a blood transfusion for at least twelve months, and the remaining ones experienced a significant reduction in their transfusion needs.
Collaborative Effort for Global Impact
The partnership between Vertex and CRISPR Therapeutics, with headquarters in the US and Switzerland, has led to the production of Casgevy. Around 2,000 patients in the UK are now eligible for this potentially life-changing treatment. Vertex Managing Director Reshma Kewalramani considered it a "historic day in science and medicine," while CRISPR Therapeutics CEO Samarth Kulkarni saw this as just the beginning of many applications of this method to benefit patients with serious diseases.
Utilizing the revolutionary CRISPR gene-scissor technology, Casgevy offers patients a new hope in overcoming the painful, life-long consequences of sickle cell disease and beta thalassemia. Its clinical trial results demonstrate promising symptom reduction and transfusion independence, suggesting further advancements in the field of genetic medicine for incurable genetic disorders.
Source:
Enrichment Data:
CRISPR/Cas9 gene editing technology transforms the treatment of sickle cell disease (SCD) and beta-thalassemia with Casgevy (exagamglogene autotemcel). This revolutionary therapy involves modifying the patient's own hematopoietic stem cells (HSPCs) outside the body (ex vivo). Here's a detailed explanation of the process and its effectiveness rates in clinical trials:
Treatment Process
- Cell Collection: Patients undergo bone marrow aspiration to collect stem cells.
- CRISPR Editing: The CRISPR/Cas9 system targets and edits the BCL11A gene in the HSPCs. The intent is to reactivate fetal hemoglobin (HbF) production, which enhances red blood cell function and reduces sickling and blockage risks associated with SCD and beta-thalassemia[1][2][4].
- Cell Transplantation: The edited stem cells are then reinjected into the patient. This rejuvenates healthy red blood cell production, reducing the need for blood transfusions and alleviating symptoms associated with these conditions[1][2][4].
Effectiveness Rates
- Sickle Cell Disease (SCD):
- Clinical Trials: The CLIMB-121 trial for SCD revealed promising results, with 28 patients experiencing no vaso-occlusive crises (VOCs) and no hospitalizations for at least a year, indicating a substantial reduction in disease complications[2].
- Transfusion Independence: Over 90% of treated patients remained transfusion-independent for more than a year, post-gene therapy[1].
- Beta-Thalassemia:
- Clinical Trials: Positive outcomes emerged for patients receiving the treatment, with numerous becoming transfusion-independent. In 2021, several maintained stable hemoglobin levels for over a year following the procedure, marking a notable milestone in genetic medicine[1].
- Transfusion Independence: Approximately 85% of participants achieved transfusion independence[1].
Summary
Casgevy, an application of the CRISPR/Cas9 technology, represents a novel and transformative therapy for patients with SCD and beta-thalassemia. Its effectiveness rates in clinical trials are impressive, with over 90% of SCD patients and more than 85% of beta-thalassemia patients achieving transfusion independence. These results suggest the potential of CRISPR gene editing to change the landscape for incurable genetic disorders.